The word “Fracture” implies broken bone. A bone fracture happens completely or partially by trauma due to a fall, motor vehicle accident, or sports. Thinning of the bone due to osteoporosis in the elderly can cause the bone to break easily. An overuse injury is a common cause of stress fractures in athletes. Here we share some light over the subject ‘Types of Fractures’.
Types of fractures
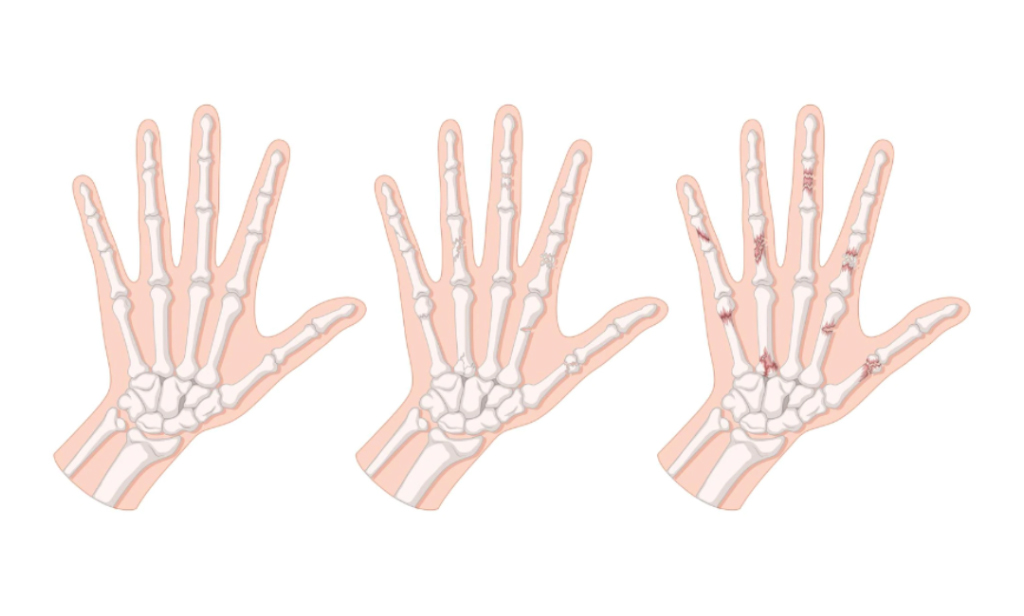
Simple fractures
In this type of fracture, the pieces of bone do not have alignment problems and are stable too.
Unstable fractures
Those fractures in which fragments of the broken bone are misaligned and displaced.
Open (compound) fractures
Severe fractures in which the broken bones cut through the skin. This type of fracture is more prone to infection and requires immediate medical attention.
Greenstick fractures:
This is a unique fracture in children that involves bending one side of the bone without any break in the bone.
Fracture Healing
Our body reacts to a fracture by protecting the injured area with a blood clot and callus or fibrous tissue. Bone cells begin forming on either side of the fracture line. These cells grow towards each other and thus close the fracture.
Medical Therapy
The objective of early fracture management is to control bleeding, prevent ischemic injury (bone death) and to remove sources of infection such as foreign bodies and dead tissues. The next step in fracture management is the reduction of the fracture and its maintenance. It is important to ensure that the involved part of the body returns to its function after the fracture heals. To achieve this, maintenance of fracture reduction with immobilization technique is done by either non-operative or surgical methods.
Non-operative (closed) therapy
Non-operative (closed) therapy comprises casting and traction (skin and skeletal traction).
Casting
Closed reduction is done for any fracture that is displaced, shortened, or angulated. Splints and casts made up of fiberglass or plaster of Paris material are used to immobilize the limb.
Traction
The traction method is used for the management of fractures and dislocations that cannot be treated by casting. There are two methods of traction namely, skin traction and skeletal traction. Skin traction involves the attachment of traction tapes to the skin of the limb segment below the fracture. In skeletal traction, a pin is inserted through the bone distal to the fracture. Weights will be applied to this pin, and the patient is placed in an apparatus that facilitates traction. This method is most commonly used for fractures of the thigh bone.
Surgical Therapy
Open Reduction and Internal Fixation (ORIF)
This is a surgical procedure in which the fracture site is adequately exposed and reduction of fracture is done. Internal fixation is done with devices such as Kirschner wires, plates and screws, and intramedullary nails.
External fixation
External fixation is a procedure in which fracture stabilization is done at a distance from the site of fracture. It helps to maintain bone length and alignment without casting. External fixation is performed in the following conditions:
- Open fractures with soft-tissue involvement
- Burns and soft tissue injuries
- Pelvic fractures
- Comminuted and unstable fractures
- Fractures having bony deficits
- Limb-lengthening procedures
- Fractures with infection or non-union
Rehabilitation
Fractures may take several weeks to months to heal completely. You should limit your activities even after the removal of the cast or brace so that the bone becomes solid enough to bear stress. The rehabilitation program involves exercises and a gradual increase in activity levels until the process of healing is complete.
Growth Plate Fractures
Growth plates, also called the epiphyseal plate or physis, are the areas of growing cartilaginous tissue found at the ends of the long bones in children. These growth plates determine the length and shape of the mature bone. The growth plates are more susceptible to damage from trauma because they are not as hard as bones. Growth plate injuries commonly occur in growing children and teenagers. In children, severe injury to the joint may result in a growth plate fracture rather than a ligament injury. Any injury that can cause a sprain in an adult can cause a growth plate fracture in a child. Growth plate fractures are more common in boys than girls because the plates develop into mature bone faster in girls.
Types of growth plate fractures
Growth plate fractures can be classified into five categories based on the type of damage caused.
Type I – Fracture through the growth plate
The epiphysis is separated from the metaphysis with the growth plate remaining attached to the epiphysis. The epiphysis is the rounded end of the long bones below the growth plate and the metaphysis is the wider part at the end of the long bones above the growth plate.
Type II – Fracture through the growth plate and metaphysis
This type is the most common type of growth plate fracture. The growth plate and metaphysis are fractured without involving the epiphysis.
Type III – Fracture through the growth plate and epiphysis
In this type of injury, the fracture runs through the epiphysis and separates the epiphysis and growth plate from the metaphysis. It usually occurs in the tibia, one of the long bones of the lower leg.
Type IV – Fracture through growth plate, metaphysis, and epiphysis:
Type IV is when the fracture goes through the epiphysis and growth plate, and into the metaphysis. This type often occurs in the upper arm near the elbow joint.
Type V – Compression fracture through growth plate:
This type of fracture is a rare condition where the end of the bone gets crushed and the growth plate is compressed. It can occur at the knee or ankle joint.
Causes
Growth plate injuries happen due to accidental falls or blows to the limbs during sports activities such as gymnastics, baseball, or running. They may also result from overuse of tendons and certain bone disorders such as infection that can affect the normal growth and development of the bone. The other possible causes which can lead to growth plate injuries are:
- Child abuse or neglect
- Exposure to intense cold (frostbite)
- Chemotherapy and medications
- Nervous system disorders
- Genetic disorders
- Metabolic diseases
Signs and symptoms
- Inability to move or put pressure on the injured extremity
- Severe pain or discomfort that prevents the use of an arm or leg
- Inability to continue playing after a sudden injury because of pain
- Persistent pain from a previous injury
- Malformation of the legs or arms as the joint area near the end of the fractured bone may swell
In children, fractures heal faster. If a growth plate fracture is left untreated it may heal improperly causing the bone to become shorter and abnormally shaped.
Diagnosis
Your doctor will evaluate the condition by asking you about the injury and performing a physical examination of the child.
- X-ray report
- Computed tomography (CT) scan.
- Magnetic resonance imaging (MRI).
These tests are helpful in detecting the type and extent of the injury as it allows the doctor to see the growth plate and soft tissues.
Treatment
The treatment for growth plate injuries depends upon the type of fracture involved. In all cases, the treatment should begin as early as possible and include the following:
Immobilization
The injured limb covered with a cast or a splint may be given to wear. The child will be advised to limit activities and avoid putting pressure on the injured limb.
Manipulation or surgery
If the fracture is displaced and the ends of the broken bones do not meet in the proper position, then your doctor will unite the bone ends into the correct position either manually (manipulation) or surgically. Sometimes, a screw or wire may be used to hold the growth plate in place. The bone is then immobilized with a cast to promote healing. The cast is removed once healing is complete
Physical therapy
You can start exercises such as strengthening and range of motion only after the healing of the fracture. Do these to strengthen the muscles and improve the movement of the joint. A physical therapist will design an appropriate exercise schedule for your child.
Long-term follow-up
We need periodic evaluations to monitor the child’s growth. Evaluation includes X-rays of matching limbs at intervals of 3 to 6 months for at least 2 years. Most growth plate fractures heal without any long-term problems. Rarely, the bone may stop growing and become shorter than the other limb.
Non-unions
Treatment of fractures involves the joining of the broken bones either by immobilizing the area and allowing the bone to heal on its own, or by surgically aligning the broken bones and stabilizing them with metal pins, rods, or plates. Sometimes, the broken bone fails to re-join and heal even after treatment. This is non-union. Non-union occurs when the broken bones do not get sufficient nutrition, blood supply, or adequate stability (not immobilized enough) to heal. Identify non-union by pain. After the initial fracture pain gets relief, swelling, tenderness, deformity, and difficulty bearing weight.
Non-surgical treatment
This method involves the use of a bone stimulator, a small device that produces ultrasonic or pulsed electromagnetic waves, which stimulates the healing process. The doctor will instruct you to place the stimulator over the region of non-union for 20 minutes to a few hours every day.
Surgical treatment
- Implanting metal rods, plates, or screws.
- Healthy blood supply at the fracture site
- Bone grafts
Stress Fractures
A stress fracture is a small crack in the bone that occurs from an overuse injury of a bone. It commonly develops in the weight-bearing bones of the lower leg and foot. Overworking or stress on the muscles of the foot causes the muscles to transfer the stress to the bone which results in stress fracture. Stress fractures are caused by a rapid increase in the intensity of exercise. Impact on a hard surface, improper footwear, and increased physical activity.
Treatment
Treating stress fractures includes rest and limiting the physical activities that involve the foot and ankle. If children return too quickly to the activity, it may lead to chronic problems such as harder-to-heal stress fractures. Doctors recommend protective footwear which helps to reduce stress on the foot. Your doctor may apply a cast to the foot to immobilize the leg which also helps to remove the stress. The use of crutches is advisable to heal the stress fracture completely. Surgery may be required if the fracture is not healed completely by non-surgical treatment.
Measures to prevent stress fractures:
- Ensure to start any new sports activity slowly and progress gradually
- Cross-training
- Ensure a healthy diet with calcium and vitamin D-rich foods.
- Ensure that your child uses proper footwear
Conclusion
In case you notice any symptoms in your neighborhood it is suggestable to contact a doctor immediately and take the help of a specialist like an orthopedic surgeon or you can contact us.
Dr. Abhinav Bhatnagar did his post-graduation from the prestigious Bangalore Medical College, Banglore after completing his M.B.B.S from Nagpur. He then completed his DNB from Fortis Hospital, Mumbai where he received the Star Student of the year award in Orthopedics. Also, did a fellowship in Hip & Knee replacement in Mumbai followed by Knee & Shoulder Arthroscopy & Sports Injuries fellowship in Pune. The doctor has authored more than 10 papers in national and international journals. He has been selected for a traveling fellowship to the U.K. in Arthroscopy & Sports Injuries. He is now a full-time Consultant Orthopaedic Surgeon at Abhinav Multispeciality Hospital, Nagpur, and visiting Consultant at Aditya Hospital, Ramdaspeth (9:00 am–11:00 am) & Mure Memorial Hospital, Sitabuldi (11:00 am–12:00 pm).